The author of the article
Boris Lipovetskiy, DMD, 31 years experience
Some patients believe that dental implants are unnecessary if the missing tooth is not visible when smiling. However, after losing a tooth, bone loss in the mouth begins.
In this article, we'll explain what jawbone loss is, potential complications of leaving it untreated, and how it can be treated.
What Is Jaw Bone Loss?
Bone resorption or atrophy refers to the decrease in bone volume and density.
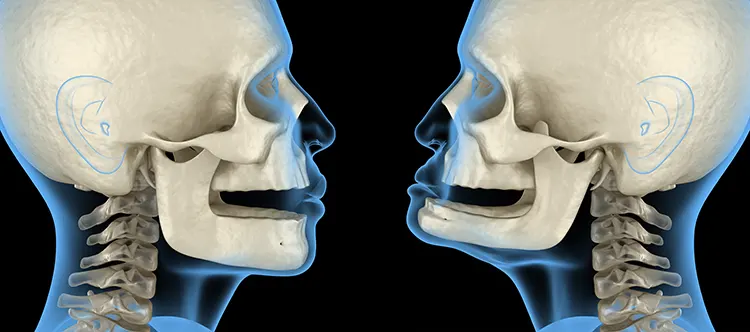
- How Does Osteoporosis Progress? Often, bone loss in the jaw begins after a tooth is extracted or lost. The tissue surrounding the tooth no longer receives the necessary load. Additionally, the supply of nutrients (minerals delivered through blood vessels in the tooth) decreases. As a result, the bone loses density and resorbs, leading to a reduction in its size.
- How Quickly Does Bone Deteriorate? Within a year after losing a tooth, the bone in that area can shrink by up to 25% (one quarter). Hence, it is important to receive treatment as soon as possible, in order to prevent deterioration. An implant or bone graft are two solutions that we offer in cases of bone loss. Grinding and crunching contribute to bone loss, and the damage can often lead to a bacterial infection, such as periodontitis. This emphasizes how crucial it is to have a proper brite.
The jawbone consists of three types of tissue:
1. Cortical (Outer) Layer: This layer is strong and protects the inner layers of the jaw. It is difficult to break down but lacks regenerative cells (osteoblasts), resulting in very slow regeneration.
2. Trabecular (Spongy) Layer: This porous and more fragile layer provides tissue nutrition, rapid recovery, and absorbs the load during chewing.
3. Basal (Deep) Layer: The most robust tissue in the jaw, which is almost unaffected by atrophy.
Each patient has different proportions of these bone tissue layers. If the outer or deep layer predominates, the jaw atrophies more slowly. If the spongy layer predominates, tissue breakdown occurs more quickly and is more noticeable.
Causes of Bone Loss
-
Loss of One or More Teeth: Without sufficient nutrition and load, the bone deteriorates.
-
Gum Disease: Chronic inflammation leads to the production of proteins and enzymes that gradually destroy the bone.
-
Injuries: Fractures or cracks in the jaw disrupt blood circulation, slowing down bone nutrition and leading to gradual deterioration.
-
Systemic Diseases: Conditions such as osteoporosis, osteopenia, and hormonal imbalances increase bone fragility and destruction.
-
Genetic Factors: A hereditary predisposition to slow tissue nutrition, fragility, and rapid bone deterioration.
-
Age: Older patients experience slower recovery from damage and an increased risk of accelerated bone loss.
Doctor's opinion
At our clinic, we see patients with varying degrees of bone loss in the mouth. To prescribe appropriate treatment, the doctor conducts a thorough diagnosis.
An essential part of treating atrophy in the absence of one or more teeth is the placement of dental implants.
If implantation is not performed in the early stages of atrophy, complications may arise. In such cases, treatment will be more complex and more expensive.


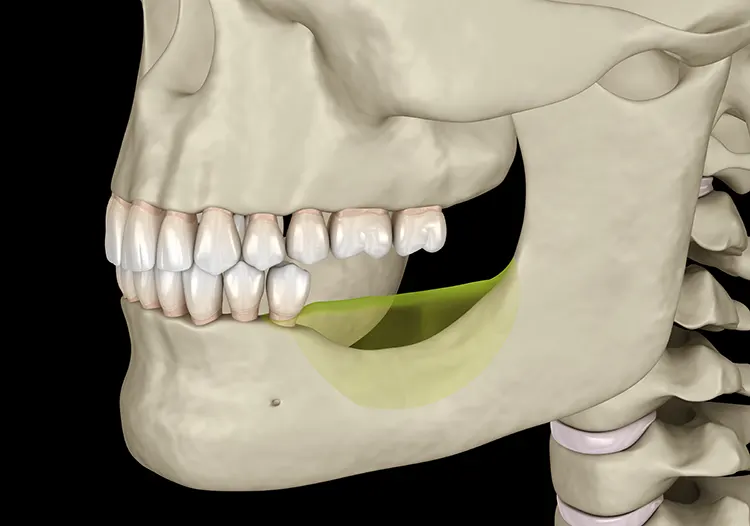
Description: Due to the absence of teeth, the jawbone started to shrink. This resulted in facial and smile asymmetry, deepened wrinkles, and problems with the temporomandibular joint (TMJ).
Treatment: Dr. Boris Lipovetsky conducted a thorough diagnosis. Since the atrophy was in its early stages, he placed zirconia implants without performing bone grafting. Zirconia crowns were also applied to the lower teeth with worn enamel.
Results: The bite improved, the smile and facial features became more symmetrical, wrinkles smoothed out, and TMJ symptoms (headaches, back pain) disappeared.
How Can You Identify Symptoms of Jawbone Loss?
- Loose Teeth: When the bone deteriorates, tooth roots lose their support, causing teeth to become loose.
- Poor Denture Fit: Removable dentures rely on the bone for support. If a gap forms between the denture and the jaw, it may start to rub, causing discomfort. This likely indicates a change in the size of the bone ridge.
- Receding Gums: Bone loss in the jaw can cause the gum line to recede, exposing the roots of the teeth. This may increase sensitivity to cold, hot, sweet, and salty foods.
- Accelerated Aging: Moderate to severe bone resorption reduces the height of the lower third of the face. Lips may appear sunken, and wrinkles deepen, making the patient look older than their age.
Types of Bone Loss
Dentists classify bone loss in the jaw by its extent:
- Minor – Almost unnoticeable. Pathology can only be diagnosed through an X-ray. Osteoplasty is not needed for treatment.
- Moderate – Teeth may become loose, and denture fit may be compromised. Bone grafting is often necessary before implantation to ensure the implant is securely anchored in the jaw.
- Severe – Highly noticeable. One or more seemingly healthy teeth may fall out. Implant placement is nearly impossible without bone grafting.
Diagnosis
- Examination and Medical History: The doctor evaluates if any teeth are missing, whether the remaining teeth are loose, and if there is any inflammation or gum recession. They also look for facial asymmetry and ask the patient about their symptoms.
- X-ray Imaging: X-rays provide a clear view of the extent of bone loss. Even minor atrophy can be detected through this method.
How to Treat Bone Atrophy
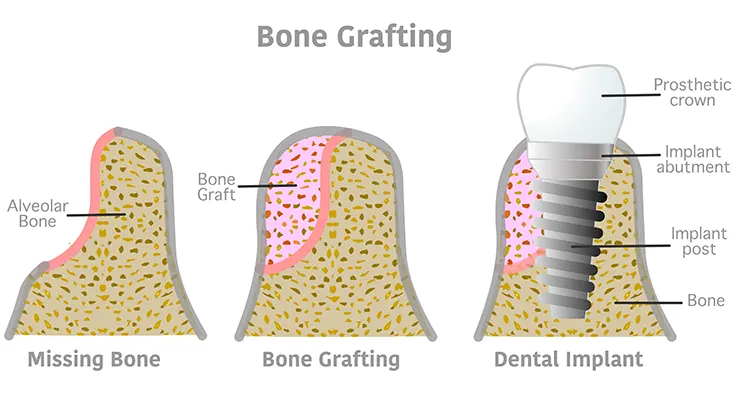
If the degree of atrophy is moderate or severe and one or more teeth are missing, the doctor will recommend osteoplasty. There are several types of procedures:
- Bone Grafting with Substitute Material. For minor bone loss, the doctor fills the gaps with bone chips or granules that replace the lost bone tissue, securing the material with a membrane. The healing process takes 3-6 months.
- Ridge Split Grafting. If the bone ridge is narrow, the dentist makes an incision in the middle and inserts a block of bone substitute material into the created space. The healing process takes about 6 months.
- Sinus Lifting. This procedure increases the volume of the upper jaw and can be either open or closed. In both cases, the height of the bone ridge is increased by using the maxillary sinuses located above the tooth row.
Implantation is typically performed only after the bone substitute material has healed, usually 3-6 months after osteoplasty.
Dental Implants for Bone Loss
Missing Multiple Teeth
When a patient loses one or two teeth, early bone atrophy can occur due to the lack of stimulation to the jawbone.
- Single Tooth Implant: A titanium or zirconia implant is placed into the jawbone to replace the missing tooth root. After integration with the bone, it provides a stable base for a crown.
- Implant-Supported Bridge: This is used when two or more adjacent teeth are missing. Implants are placed at both ends of the gap to support a bridge made of ceramic or zirconia.
Doctor's opinion
When early bone atrophy occurs, dental implants are the best solution because they help prevent further bone loss and restore the functionality of teeth. Once the implant integrates with the bone, it helps maintain the structure of the jaw.
Key Advantages:
-
Stability: Implants provide a strong foundation, preventing prosthesis movement
-
Bone Preservation: By distributing chewing forces, implants help maintain remaining bone and stimulate new bone growth
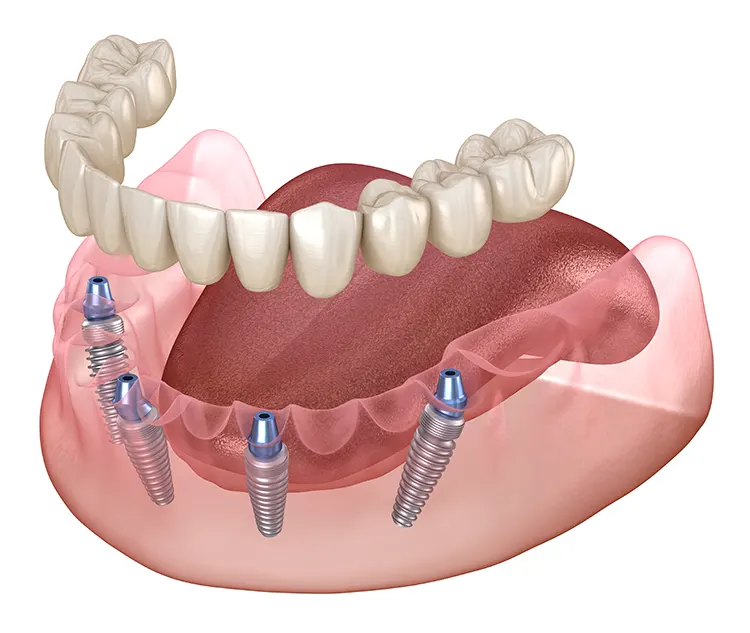
Complete Tooth Loss in One Jaw
For patients who have lost all teeth in one jaw, progressive bone atrophy is a common issue.
-
All-on-4 Implants
The All-on-4 method uses four strategically placed implants to support a full arch of teeth. This approach is particularly beneficial for patients with significant bone loss:
• Angled Implants: Two implants are placed at an angle to increase bone contact, providing stability even in areas with lower bone density.
• Minimally Invasive: This method often requires less bone grafting than traditional implants, making it suitable for patients with moderate to severe bone loss.
• Immediate Function: All-on-4 implants can often support a temporary prosthesis on the same day as the surgery, allowing patients to quickly regain functionality.
-
All-on-6 Implants
The All-on-6 method uses six implants to support a full arch, offering even greater stability and support than the All-on-4:
• Additional Implants for Stability: The two extra implants provide additional support, evenly distributing chewing forces across the jaw.
• Utilization of Bone Tissue: Like All-on-4, All-on-6 implants are placed in areas of highest bone density, minimizing the need for bone grafting.
• Increased Durability: The additional implants enhance the strength and longevity of the prosthesis, making it ideal for patients with significant bone atrophy.
Why Is Bone Loss in the Mouth Dangerous?
If atrophy is not treated, it will progress and lead to complications:
- Tooth Loss: Due to compromised root stability, teeth can fall out completely.
- Prosthesis Dislodgement: As the bone ridge diminishes, removable dentures fit poorly, increasing the risk of them falling out during eating or speaking.
- Facial Asymmetry: Reduction in jaw volume disrupts facial proportions, leading to noticeable aging with deep wrinkles, a receding chin, and sunken lips.
- Difficulty Chewing: Missing teeth make it challenging to bite and chew food, especially harder items.
- Bite Misalignment: When teeth are lost, adjacent teeth shift to fill the empty space, causing improper jaw alignment.
- TMJ Problems: Uneven chewing forces affect the temporomandibular joint, leading to clicking sounds, pain while opening and closing the jaws.
Prevention of Bone Loss
- Regular Brushing: Maintain thorough oral hygiene to prevent gum diseases, which increase the risk of jawbone atrophy.
- Regular Dental Visits: Regular check-ups allow the dentist to detect pathologies and bone loss in the jaw early and prescribe appropriate treatment.
- Prompt Tooth Replacement: If you lose a tooth, consult a dentist for an implant as soon as possible to prevent critical bone loss.
FAQ
Yes, dental implants can be placed even with bone loss. However, a thorough diagnosis is necessary to determine the appropriate placement method and whether bone grafting is needed.